Editor’s note: A version of this article originally appeared on the Frederick National Laboratory website.
After three years of COVID-19, science has learned much about the disease and the virus that causes it, SARS-CoV-2. But in the bigger biological and clinical picture, there are still many unanswered questions, says Ligia Pinto, Ph.D.
That’s what keeps her group, the Vaccine, Immunity, and Cancer Directorate at Frederick National Laboratory, working hard to hunt down answers.
Now, they and collaborators in FNL’s Protein Expression Laboratory, the National Cancer Institute, and the National Institute of Allergy and Infectious Diseases have filled in another gap in that bigger picture. They’ve published an in-depth look at IgG antibodies to the SARS-CoV-2 spike protein after infection or mRNA vaccination. The study, which appears in Human Vaccines & Immunotherapeutics was conducted across 310 samples drawn from a combination of unvaccinated and vaccinated participants.
The results not only confirm what scientists knew to be true—that vaccination produces higher antibody levels and more potent antibodies against this coronavirus than infection—they give specific standardized numbers and measurements.
Notably, vaccinated persons had nearly 10 times more SARS-CoV-2 IgG antibodies than naturally infected people on average, and the vaccinated group’s antibody avidity response—binding strength to SARS-CoV-2—was approximately 1.4 times greater than the naturally infected group. One month after the primary vaccination series, antibody avidity responses were greater in participants who received the Moderna vaccine than the Pfizer vaccine across all age groups, the team reported.
Antibody levels dropped precipitously by four months after vaccination (the cutoff for the study). Despite this, the antibodies had greater binding at the four-month mark than when participants received the vaccine. This information aligns with what scientists suspected, helps them understand how the immune system responds to mRNA vaccines, and aids in efforts to evaluate future vaccines, the team reported.
“The main finding is that the vaccination induced a very strong immune response early on, and then there was a significant decay of the response developed after the primary vaccination series, and this is one of the reasons why the boosters became necessary,” Pinto said.
Additional studies seeking to identify antibody levels and potency after booster vaccination are underway.
‘Plug-and-play’ Approach, Expertise Enable Standardized Results
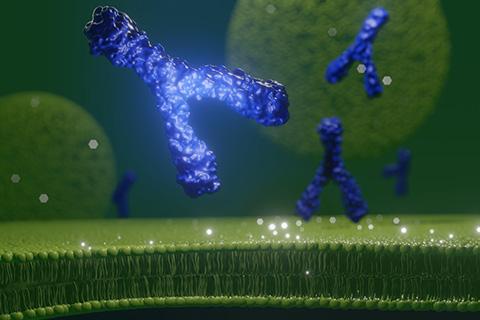
IgG antibodies have become the primary focus of the search for immunity to SARS-CoV-2. They’re what most often come to mind at the mention of “antibody”: the archetypal, Y-shaped molecular security guards ready to intercept intruders. In the case of SARS-CoV-2, they’re a key player in preventing infection by attaching to the spike protein on the surface of the virus.
But “no one knows what is the minimal amount needed for protection,” Pinto said. That’s one of the reasons studies like this, and ones that examine antibody responses in context of breakthrough infections, can be helpful.
The team used standardized assays to measure the antibody levels and antibody binding strength, which Pinto says is crucial for the findings to be relevant to inform public health decision-making. Having results tied to a standard—in this case, the U.S. Serology Standard—means any other group using the same standard and type of assay can achieve comparable results. It lets laboratories use the same benchmark.
“When you want to do something more in the clinical space and something that's more reproducible and rigorous, really, we need to have the standardized and validated assays,” said Pinto, whose laboratory also developed the U.S. Serology Standard.
Deploying standardized assays for SARS-CoV-2 antibodies was as simple as “plug-and-play,” Pinto said. Her laboratory has long worked on similar assays for human papillomavirus (HPV). Pivoting them to the coronavirus involved switching from an HPV antigen—a part of the virus that antibodies detect—to a SARS-CoV-2 antigen, in this case the spike protein. A few minor tweaks later, and the team was ready to go.
That capability is a recognized and respected part of the laboratory’s reputation at FNL, and it’s one of the achievements Pinto appreciates about her team. She sees them as an innovative, agile, committed group who are together doing their best to make a difference.
“I’m very fortunate to have a great team. Everybody is working together really hard to try to contribute in one way to mitigate the pandemic and to, really, eliminate the pandemic. So [we have a] very passionate and driven team,” she said.
Samuel Lopez leads the editorial team in Scientific Publications, Graphics & Media (SPGM). He writes for newsletters; informally serves as an institutional historian; and edits scientific manuscripts, corporate documents, and sundry other written media. SPGM is the creative services department and hub for editing, illustration, graphic design, formatting, multimedia, and training in these areas.