A task force led by physicians from the American College of Cardiology and the American Heart Association has released new blood pressure guidelines in order to help doctors and clinicians better treat hypertensive and prehypertensive individuals who may be at risk of heart disease.
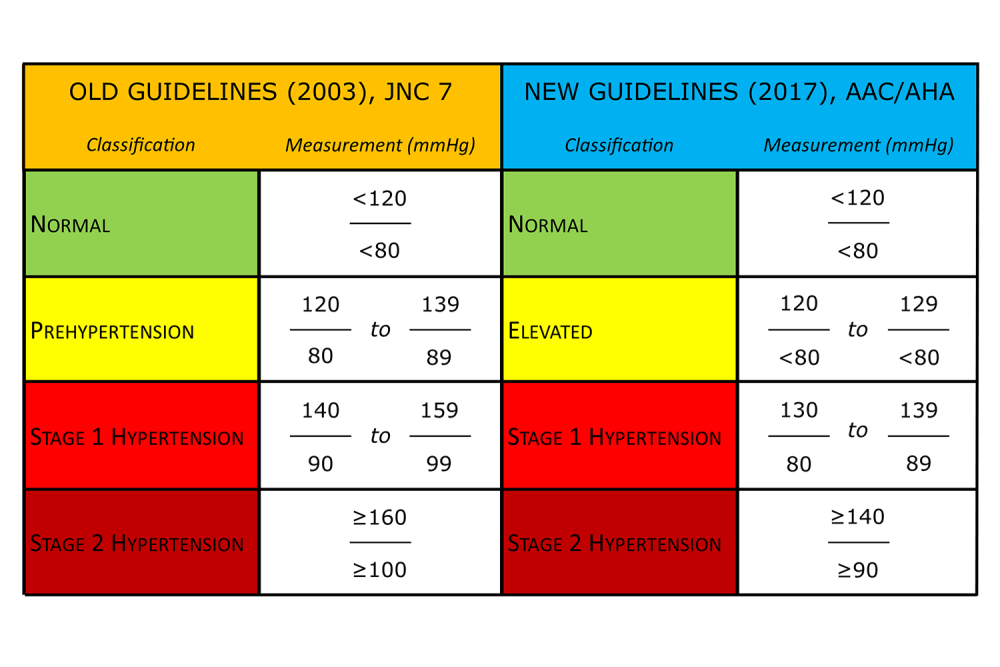
The update, which comes nearly 15 years after its predecessor, has significantly broadened the definition of hypertension and reclassified other blood pressure categories. Under the previous guidelines, individuals were considered hypertensive if their blood pressure was at least 140/90. Now, the number is 130/80.
According to the task force’s report, the new clinical guidelines are based on scientific evidence and observational data regarding blood pressure and the risk of cardiovascular disease. Studies like the American College of Cardiology’s Systolic Blood Pressure Intervention Trial (SPRINT) have also shown that lowering blood pressure can help reduce mortality rates in older adults, who, along with other at-risk groups such as diabetics and prehypertensive individuals, are intended to be the main beneficiaries of the new guidelines.
“They took the previous prehypertension values and changed them to hypertension because this category of patients was already at double the risk for cardiovascular complications,” said Sarah Hooper, manager, Occupational Health Services (OHS), NCI at Frederick.
Hooper added that, while the guidelines are rigorous, they are “pragmatic” and aim to “help empower people to make changes and lower their risk for heart disease.” She believes that the guidelines may alter some aspects of healthcare in the United States, especially when and how often doctors prescribe antihypertensive medication. However, that means doctors will also have more responsibility to manage their patients’ medications and monitor blood pressure.
For NCI at Frederick employees, Hooper says that’s where OHS can help.
“Everyone knows someone who goes into the doctor’s office and automatically has elevated blood pressure, so it is important to have accurate readings outside of the physician’s office,” she said. “[We can] contribute to the employee by augmenting care with out-of-office or different-setting [blood pressure] data.”
Employees can schedule an appointment with OHS to have their blood pressure measured, or they can simply attend OHS’ walk-in blood pressure clinic from 12:00–12:30 p.m. on Tuesdays and Thursdays. The trained medical staff are up to date with the latest guidelines and measurement practices, but they try to provide a more relaxed atmosphere so employees won’t feel uncomfortable. If an employee does test positive for elevated or hypertensive blood pressure, the staff will recommend that they follow up with their personal physician.
In addition, “an employee can bring in their home blood pressure monitoring equipment to determine if it obtains readings that are similar to or in alignment with the readings that are obtained by the experienced staff,” said Hooper.
In the meantime, Hooper encourages employees with high blood pressure to follow the American Heart Association’s five steps for lowering it: maintaining a healthy weight (body mass index between 18.5 and 24.9); eating less saturated fat and more fruits, vegetables, and low-fat dairy; reducing sodium intake; doing 90–150 minutes of aerobic exercise per week; and limiting alcohol consumption.
And of course, if employees aren’t sure about their blood pressure, they can always visit OHS.