As the director of the Molecular Diagnostics Laboratory, Gordon Whiteley has one message for his team: “Treat every sample as if it were your own, your mother’s, or (from) someone you care about.”
Whiteley and his team, part of the Cancer Research Technology Program at the Frederick National Laboratory, work in a high-complexity lab at the Advanced Technology Research Facility that operates under rigorous standards of the Clinical Laboratory Improvement Amendments (CLIA). The tests developed by the lab (one of five high-complexity labs associated with FNL) generally are not available anywhere else.
The lab often works with investigators from the National Cancer Institute who need to test a new medication so it can clear preclinical hurdles and assist scientists at the NIH Clinical Center to develop tests that can determine whether patients qualify for an existing drug. They also conduct assays for researchers at the National Institute of Allergy and Infectious Diseases (NIAID).
As the only lab at the ATRF which produces test results that may be shared with physicians, patients, or patients’ families for disease diagnosis, prevention, or treatment, federal regulations require that the lab be CLIA compliant.
The rigorous CLIA standards are critical, given the implications of the tests being done by the Molecular Diagnostics team. For instance, the lab offers a test for genes related to transporters and enzymes involved in the metabolism of chemotherapy drugs to determine correct dosing standards. The test is critical because every patient is unique and may metabolize the drug differently. A dose that may be therapeutic to some patients could be potentially toxic for others.
Centers for Medicare and Medicaid Services (CMS) inspectors want to see that CLIA labs are following strict standard operating procedures for any assay or workflow being performed. This includes documenting accuracy, precision, reportable range, reference range, analytical sensitivity, and analytical specificity.
“The development of a test is a rigorous process,” said Kristen Pike, associate scientist for the CLIA Molecular Diagnostics Lab. “We determine the quality metrics for a test, the parameters, and the controls to run.”
And in situations where controls, reagents, samples, or instruments fail, the lab must investigate and document what went wrong and note its corrective actions.
Whiteley’s seven-person team includes scientists, technicians, and a genomics consultant who are required to follow strict CLIA protocols, undergo rigorous training and evaluation programs, and keep copious documentation.
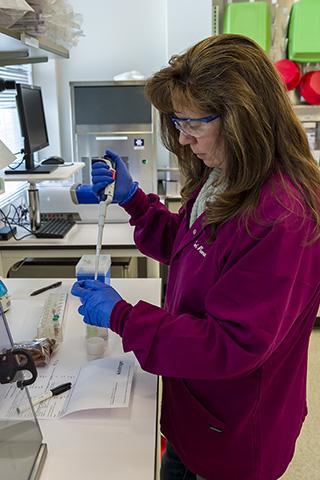
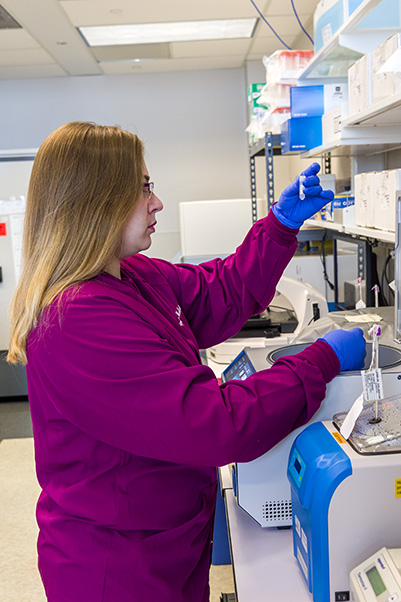
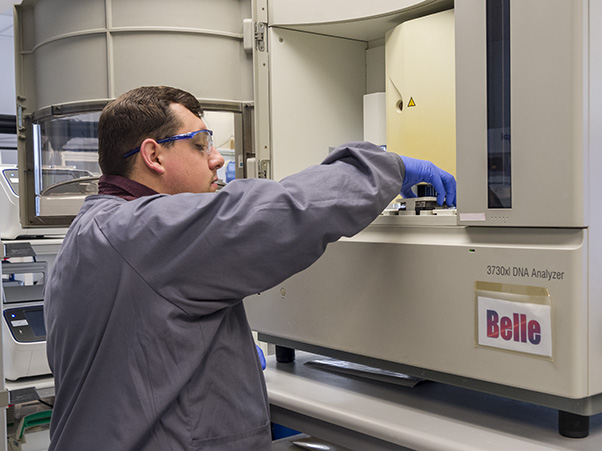
All equipment used in patient testing procedures must be calibrated to National Institute of Standards and Technology (NIST)–traceable standards every six months (unless otherwise covered by manufacturer’s service agreement). This includes devices as simple as pipettes and thermometers all the way up to balances, spectrophotometers, PCR machines, ovens/incubators, rotators/mixers, centrifuges, heat blocks, DNA sequencers, biosafety cabinets, microarray scanners, and liquid handling robots.
“We can’t just purchase a new instrument, plug it in, and start running patient samples on it,” Pike said.
Reagents bottles and vials must be labeled with the date received, date opened, receiver’s and opener’s initials, and expiration date. That information must be also be documented in a logbook, as are daily temperatures and equipment maintenance. Protocols must be locked, versioned, include all precautions and procedures, and specimens must be assigned unique CLIA Molecular Diagnostics Laboratory identification numbers. All documentation is then reviewed, and ultimately signed and dated by Whiteley. Bi-weekly CLIA meetings and quarterly quality assessment reviews are also conducted by the group.
Lab technicians who are running tests every day must pass an initial competency evaluation. Six months later, they are required to pass another review and are then assessed annually. On top of that, every assay also must be tested every six months for proficiency. That’s a lot of proficiency reviews given that the lab has assays for more than 85 genes that use traditional PCR and Sanger sequencing. It also has assays for 225 other genes that employ other technologies such as DMET microarrays and Nanostring. And they plan to add CLIA-validated Droplet Digital PCR (ddPCR), Pharmacoscan, RNAScope, Mass spectrometry and Real-Time PCR in 2020.
“We are assessing someone’s competency or some assay’s proficiency year-round,” Pike said.
Once granted, the lab’s CLIA certification lasts for two years, but Whiteley says his team must be ready at any time for an inspection by CMS. “Although we normally get a heads-up, under the law they could be downstairs right now and say, ‘We want to come up and look at all of your documents,’” he said.
Despite the stringent CLIA requirements, Pike says gaining recertification is not difficult—provided that protocols are followed every day.
“It all goes back to quality,” she said. “When you write your standard operating procedures, say what you are going to do, what tests you are going to run, and how you are going to run them. Then you need to stick to that. The inspectors want to see an effort to process samples in a timely manner, but also with quality and accuracy.”
Pike advises those who might be considering CLIA certification for their labs to give themselves ample lead time to prepare. “It takes several months to get appropriate staffing, equipment, and assay testing up and running,” she said.
As a diplomate of the American Board of Medical Microbiology who has extensive experience in the clinical microbiology and chemistry lab fields, Whiteley knows better than anyone that adhering to CLIA regulations—all 400 or so pages of them—may be exhausting at times. But it is the kind of painstaking quality control that every patient and their loved ones deserve.
“We have to make sure the test is robust,” Whiteley said. “It has to work every time before we go live with it because we don’t get second chances.”