A new advance in our understanding of HIV comes from what Steve Hughes, Ph.D., calls “an odd observation.”
Certain people living with HIV had only partially suppressed levels of virus in their blood despite being on effective antiretroviral therapy (drugs used to manage HIV). At first, an explanation seemed like it would be simple—but it wasn’t.
Doctors usually attribute the phenomenon to the two typical causes: Either the people were skipping doses of the drugs or the virus was mutating to develop resistance to the therapy. But when John Mellors, M.D., and his laboratory at University of Pittsburgh investigated, they found that some of these people were faithfully taking the antiretrovirals as prescribed.
A larger, multi-institutional study team led by Mellors then sequenced the viral RNA—HIV’s genetic material—for mutations, but there was no evidence of resistance to antiretrovirals.
The two typical reasons couldn’t explain what was going on in these unusual individuals.
“There was something else that was very intriguing about the virus in the blood: … [it] was all, or almost all, the same virus, identical in sequence,” said Hughes, chief of the Retroviral Replication Laboratory at NCI at Frederick and a senior member of the team. “It wasn’t a complex collection of viruses, which is what you often see [in people].”
That was when it clicked: The scientists realized the identical virus may come from a clone, a large, genetically identical population of cells carrying the same copy of HIV’s genetic material. They performed multiple tests that eventually confirmed the theory.
The team—scientists from the University of Pittsburgh, NCI at Frederick, Frederick National Laboratory for Cancer Research, Weill Cornell Medicine, and Tufts University—gave these cells a fitting name, “repliclone,” and identified repliclones in four people living with HIV who are taking antiretroviral therapy.
These clones are more than a curious phenomenon, too. They present a massive challenge to curing HIV.
Meet the bad guys
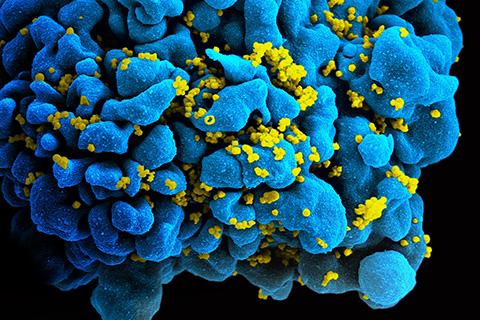
A repliclone is a family of HIV-infected white blood cells called “T cells.” They are identical daughter, granddaughter, and descendant cells derived from a single HIV-infected T cell. Some repliclones can grow to have tens of millions of identical cells.
It’s normal for T cells to make clones of themselves. One cell splits into two, and the two new cells are twins. As the cell division continues, the clone—the family—grows. This is part of how the immune system works: T cells that recognize a bacterium or virus rapidly form clones to defend the body.
The tables turn once HIV enters the mix. When the virus infects a T cell, it inserts a copy of its genetic material into the cell’s DNA. This allows it to use the cell’s biological machinery to make and release new virions that can infect new cells.
It also makes HIV a hitchhiker. Most T cells die shortly after they’re infected, but if an infected cell survives and makes a clone, the HIV DNA embedded in the cell’s DNA comes along with it. The two new daughter cells are already infected. Because every cell in a repliclone is descended from the same infected cell, they all carry an identical strain of HIV.
Most of the time, the DNA in the infected cell is defective, but repliclones are different. The HIV DNA in them is intact and correct, meaning repliclones are all capable of making virus particles. Most are dormant, but in some people, a tiny percentage of the cells leak a small but steady trickle of virus into the bloodstream, even if the people are taking antiretroviral therapy.
That’s a problem.
Antiretroviral therapy can’t fix it
In most of these people, the trickle is low, and the HIV is considered to be fully suppressed. But some people, like the four identified in the study, have repliclones that release high enough levels of virus that its presence can be detected using standard techniques.
Changing the antiretroviral therapy or adding new drugs would make little difference, the team points out. That’s because the released virus comes from cells—and descendants of cells—that were infected before the person began therapy.
Antiretroviral drugs don’t eliminate circulating virus released from repliclones—they prevent HIV from infecting new cells and using the cells to make more virus. When antiretroviral therapy suppresses HIV replication, most HIV-producing cells die off or are killed by the immune system. But therapy doesn’t prevent already-infected cells from producing HIV, nor does it prevent cells infected before therapy began from dividing and forming clones.
This is why infections come roaring back when a person goes off treatment: Antiretroviral therapy protects healthy cells from being infected. Remove the protection, and the HIV produced by repliclones can quickly begin infecting them.
In people with repliclones that produce detectable levels of virus, the problem isn’t a matter of blocking new infections—antiretroviral therapy’s territory—it’s that there are already large numbers of infected cells, some of which are producing virus particles.
“Even though you’ve stopped the virus from replicating, you haven’t stopped the infected cells from replicating, and that becomes a very important aspect of how the virus is able to persist, why the infection is able to persist,” Hughes said.
A long road to victory
Defeating the persistent infection is the key to curing HIV, but unfortunately, the discovery of the repliclones underscores how hard that will be.
A true cure must eliminate all of the infected cells that can produce HIV, which is a tall order. If just one infected cell in every thousand survives, the infection will return, Hughes says.
Destroying these cells is even harder than it sounds. In fact, it currently borders on the impossible.
The human body can’t do it alone. The immune system can recognize and eliminate the virus-producing T cells in a repliclone, but it only destroys the ones that clearly display infection. There are cells in the repliclone that don’t display that they’re infected, so the repliclone can survive and even increase in size.
On top of that, the cells with dormant viral DNA dwarf the number of cells producing virus, and they’re the silent danger. Dormant infected cells are invisible to the immune system until they awaken and start producing virus particles—and it’s not yet clear when or why they wake up.
Current methods aren’t up to the task, either. There are no means to safely and quickly detect and eliminate infected cells on a scale large enough to be effective.
Adding to the problem, the available data suggest that people have more than one repliclone, Hughes says. The one producing relatively high levels of virus is just one of the largest and most active. There are other, smaller ones that make lower levels of infectious virus.
In other words, besides this large repliclone, there are hundreds—or, Hughes says, more likely thousands—of other, different repliclones in a person. Each comprises legions of cells, some of which can also release virions.
Any potential HIV cure must therefore—to be truly safe—kill every infected cell that’s producing virus or capable of doing so, which means killing all of the cells in all of the repliclones, including the dormant, “hidden” ones. And it must do so without crippling the person’s healthy, uninfected T cells.
The technology to do that doesn’t yet exist.
“We’ve not only got to get rid of the cells that are making virus, we have to somehow approach the problem of identifying and stepping on the cells that could make virus but aren’t making virus right now, and that’s a tough nut,” Hughes said.
Piece by piece
Hughes acknowledges that while a cure remains distant, the findings move the research—and the people it seeks to help—in the right direction. New information means new ways to understand the problem, attack it, devise new technology, and create more effective treatments.
“Breaking the problem up into pieces that you can manage is the goal of the game,” he said.
Editor’s note: At NCI at Frederick, Mary Kearney, Ph.D., and team used their previously developed technology to show that the virus was coming from a small fraction of cells infected prior to initiating antiviral therapy. At the Frederick National Laboratory, Brandon Keele, Ph.D., and his laboratory performed sequencing experiments that linked the viral RNA in the blood to populations of infected cells. Wei Shao, Ph.D., helped to analyze the data and created tools for computationally estimating the intactness of the proviral DNA in infected cells. Xiaolin Wu, Ph.D., and Amber Guo, Ph.D., helped develop and implement the technologies used to show that the identical viruses in the blood came from a clone of infected cells.